Case Studies – Martha
In October 2023, Martha started limping on her left forelimb. As a 10-year-old, it was likely that osteoarthritis was the cause. It was recommended that Martha started a joint supplement and NSAIDs were discussed, which the owners facilitated. However, in November Martha deteriorated and was not weightbearing properly on that limb at all. Upon examination, it was thought there could be some nerve pain so further analgesia was added (Gabapentin and NSAID combination). The owner requested further investigation, so our orthopaedic experts worked Martha up, gaining enough evidence that there was ground to radiograph and take samples from the left shoulder joint. It was identified that a mild osteophyte (bone spur) of the caudal glenoid (the socket of the ball-and-socket shoulder joint) was present.
The sample from the joint capsule (obtained via joint-tap) and analysed in-house showed an increase in mononuclear cells which is consistent with degenerative arthropathy (joint disease).
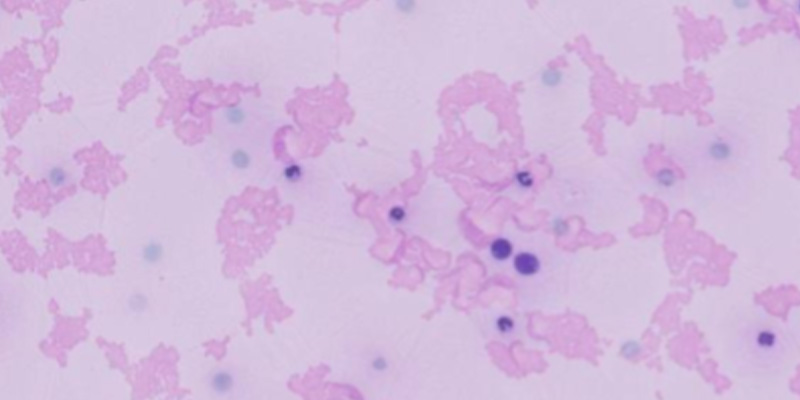
Microscope slide showing higher than expected number of mononuclear cells
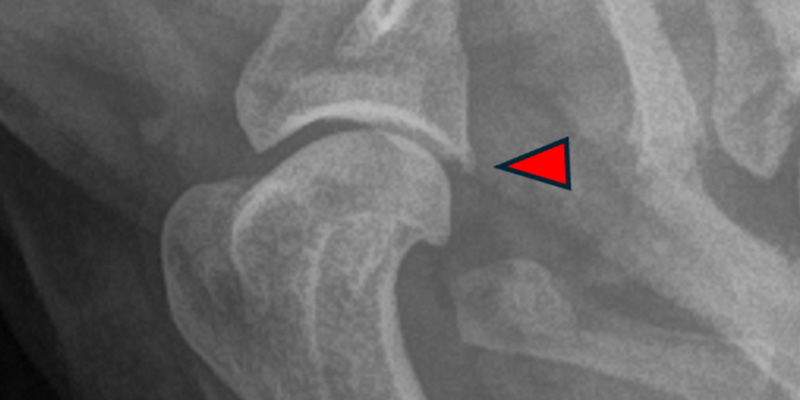
Radiograph of affected shoulder with osteophyte highlighted
Based on these findings, it was likely that the limping and non-weightbearing was caused either by a partial tear of the medial collateral ligament or a flare up of chronic arthritis. The best option for both of these differential diagnoses was for Martha to rest and continue multimodal analgesia.
Unfortunately, Martha continued to be in pain and began crying out even when lying in her bed. At re-examination, her shoulder subluxated (partially dislocated) easily and was crepitant. It was suspect therefore that the ligament’s partial tear had progressed to complete rupture. Surgery to stabilise was recommended and within a week, Martha had the procedure.
Within this, it was observed there was no significant damage to the cartilage. The surgeon placed implants which anchored the proximal humerus to the medial distal scapula. After strict rest with gentle PROM physiotherapy and hydrotherapy started 3 weeks-post operatively, Martha’s 6-week review highlighted that the lameness was much improved, she was fully weightbearing and walking well 50% more than she had been prior to referral, without the need for analgesia. Martha will return for orthopaedic examination with repeat radiographs if warranted, but in the meantime her owner reports she is doing very well and managing up to 20-minute walks without issue.
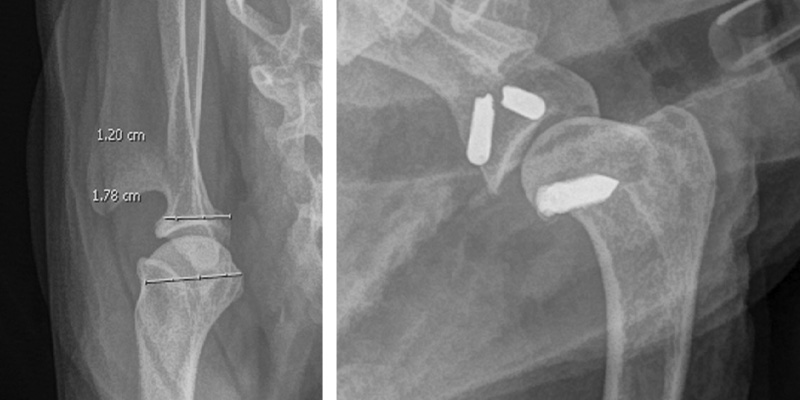
Left: pre-op measurements to establish appropriate techniques. Right: Post-op.